SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: The aim of this study was to assess the pattern of anti-atherosclerosis medicines in patients admitted to a vascular surgery department, the effective control of the target values and its subsequent modification by the vascular surgery team.
Material and Methods: A retrospective single-center cohort study of prospectively collected data was performed between May 2017 and May 2018 in a tertiary center. The STROBE guidelines were followed. All patients undergoing a primary elective surgery for carotid disease, aortic aneurysm and peripheral arterial disease were included. ‘Best medical treatment’ was defined as treatment with both anti-thrombotic and lipid-lowering treatment and, when appropriate, antihypertensive and anti-diabetic drugs. Both baseline and post-discharge best medical treatment were recorded. Blood work-up was performed at admission and ‘adequately controlled patient’ was defined if all blood test values were in agreement with the guidelines.
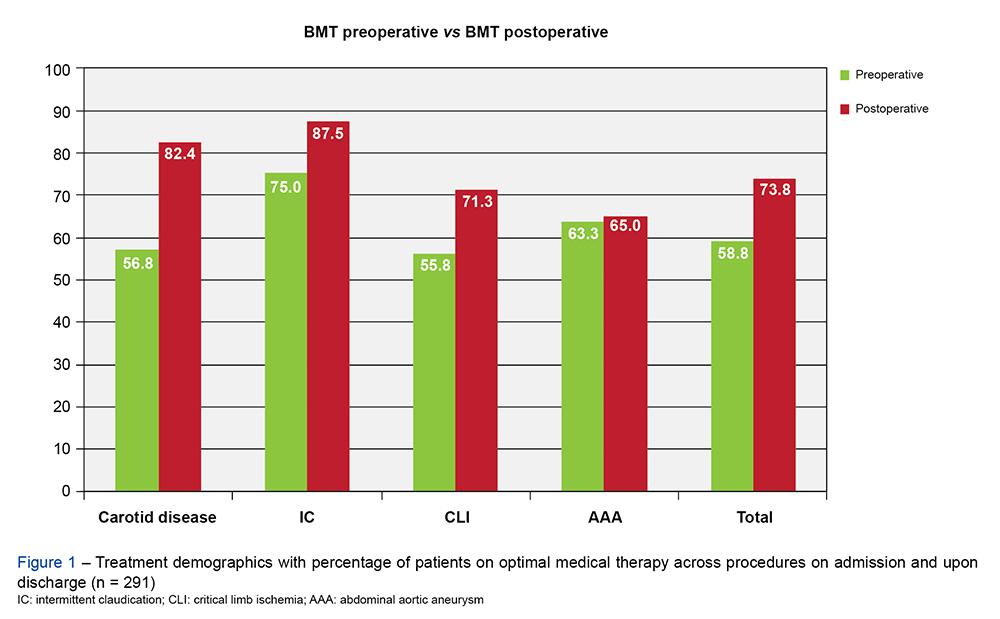
Results: A total of 279 patients (78% male; mean age 69 years-old) were included. Optimal medical therapy was registered in 58.8% upon admission but improved to 73.8% (95% CI, 2.197 – 7.781; p < 0.001) after discharge. At baseline, a total of 65.4% of patients were on lipid-lowering agents and of these, only 37% had LDL-C values within the targets. Likewise, only 34.6% of the 78 patients with diabetes had glycated hemoglobin within the normal range. Additionally, 8.5% of the remaining cohort had undiagnosed diabetes.
Conclusion: In our current practice, only 75% of the patients receive best medical treatment. Although the admission in a Vascular Surgery department was an opportunity to optimize medical therapy, treatment remains suboptimal in one-quarter of patients. Further efforts should be carried out to alert vascular surgeons to this problem and to find future multidisciplinary solutions that can improve the cardiovascular risk profiles of these patients.