SOCIAL MEDIA
Portuguese Medical Association's Scientific Journal
Introduction: Genomic assays are useful tools for tailoring adjuvant treatment in early breast cancer. We aimed to analyse the role of an institutional protocol of a genomic assay for chemotherapy de-escalation.
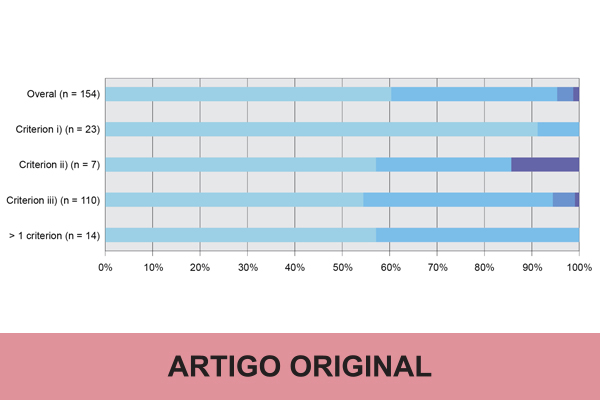
Material and Methods: Prospective cohort study of all consecutive women diagnosed with hormone receptor-positive and human epidermal growth factor receptor 2-negative early breast cancer, tested with the 21-gene Recurrence Score (RS) assay from August 2015 to July 2018 at a Portuguese cancer centre. For being tested, patients should meet at least one of the pre-defined inclusion criteria: i) luminal A-like, pT2pN0; ii) luminal A-like, 1 – 3 positive nodes and comorbidities with higher risk of chemotherapy-induced toxicity; iii) pT1-2pN0, progesterone receptor ≤ 20% and/or Ki67 14% – 40%. Adjuvant treatment was de-escalated to isolated endocrine therapy if RS was less than 18. We measured the reduction in chemotherapy prescribing and its clinical impact, the RS association with pathologic features, and the protocol feasibility.
Results: We tested 154 women with a median age of 61 years old (range: 25 – 79), 69% postmenopausal. Tumours were mainly pT1 (55%), pN0 (82%), invasive ductal (73%), G2 (86%), luminal B-like (69%) and stage IA (85%). We obtained a RS less than 18 in 60% of women, with an overall adjuvant chemotherapy reduction of 65%. Seven (95% confidence interval: 5 – 10) patients needed to be screened with the 21-gene RS assay to prevent one clinically relevant adverse event during the first six months of adjuvant treatment. Considering the currently used RS cut-off, only 9% of node-negative and 11% of node-positive patients had RS over 25. We found no relevant associations between RS and pathologic features. The protocol was feasible and did not compromise the adequate timing for adjuvant treatment.
Conclusion: These criteria allowed the de-escalation of adjuvant systemic treatment in at least six out of ten women.